ADHD, Emotions, and Exercise: Untangling the Connection
A closer look at physical activity & emotional regulation in children with ADHD
[Note: Above is an AI-generated read-through of the text summary below]
[Second note: The voiceover may pronounce “ADHD” incorrectly as “ADH.” Please disregard this—it's referring to ADHD throughout.
Also, ED refers to emotional dysregulation, a concept we review in this summary]
Attention-Deficit/Hyperactivity Disorder (ADHD) remains one of the most commonly diagnosed neurodevelopmental disorders worldwide, affecting roughly:
4–6% of children and adolescents
2.6% of adults
ADHD is marked by ongoing struggles with attention, hyperactivity, and impulsivity. It usually begins in early childhood, often before a child starts school, and can affect nearly every part of life: learning, work, relationships, and overall well-being.
People with ADHD are at increased risk for:
Mental health comorbidities
Sleep problems
Lower quality of life
Poorer outcomes in the workforce
Yet one important feature should also be included in clinical conversations: emotional dysregulation (ED).
While emotional dysregulation can occur in many psychiatric conditions, it has a particularly strong link with ADHD. For children and adolescents, emotional dysregulation may manifest as:
Intense emotional reactions
Frequent mood swings
Difficulty regulating attention when emotionally activated
These challenges often complicate social relationships, academic progress, and overall emotional development.
New Research on ADHD, Emotional Dysregulation, and Physical Activity
A 2025 study published in the Journal of Affective Disorders followed over 12,000 children into adolescence to examine the connection between early ADHD symptoms and later emotional dysregulation. Researchers also evaluated whether the frequency and intensity of physical activity affected this relationship.
They explored key questions such as:
Do early ADHD symptoms lead to emotional dysregulation in adolescence?
Do inattention and hyperactivity have different effects?
Can physical activity weaken or worsen the connection?
Researchers found that stronger ADHD symptoms in childhood predicted greater emotional dysregulation by age 15 in both boys and girls. Also, sex differences emerged:
Boys: Inattention was the primary driver of emotional dysregulation.
Girls: A combination of inattention and hyperactivity-impulsivity was more strongly associated with emotional dysregulation
There was also a significant relationship across physical activity, ADHD symptoms, and emotional dysregulation.
While physical activity didn’t eliminate the relationship between ADHD and emotional dysregulation, it did appear to influence its strength. The study measured physical activity in two ways: how often kids exercised (frequency) and how hard they exercised (intensity).
The study found that children with moderate physical activity intensity showed the strongest link between childhood ADHD symptoms and emotional dysregulation (ED) in adolescence. Despite this, they could not conclude that the effect of ADHD on emotional dysregulation is truly different based on the level of PA intensity.
They did find stronger and more consistent effects with physical activity frequency:
Low frequency of physical activity was associated with a stronger ADHD–Emotional Dysregulation link.
In boys, a low PA frequency amplified the effect of ADHD symptoms on ED.
Children with higher ADHD symptoms were also more likely to fall into low PA intensity and low PA frequency categories.
Clinical Takeaways
1. Screen for Emotional Dysregulation (ED) as part of routine ADHD assessment
Use standardized tools like:
The Strengths and Difficulties Questionnaire (SDQ): quick and easy for parents, teachers, and self-report.
The Child Behavior Checklist (CBCL) : for a more detailed behavioral profile.
Pay attention to emotional lability, frustration tolerance, and social conflict, key emotional dysregulation indicators in ADHD.
2. Assess and promote physical activity, especially frequency
Ask practical, non-judgmental questions to understand both how often and how intensely the child is active. Here are the questions researchers asked:
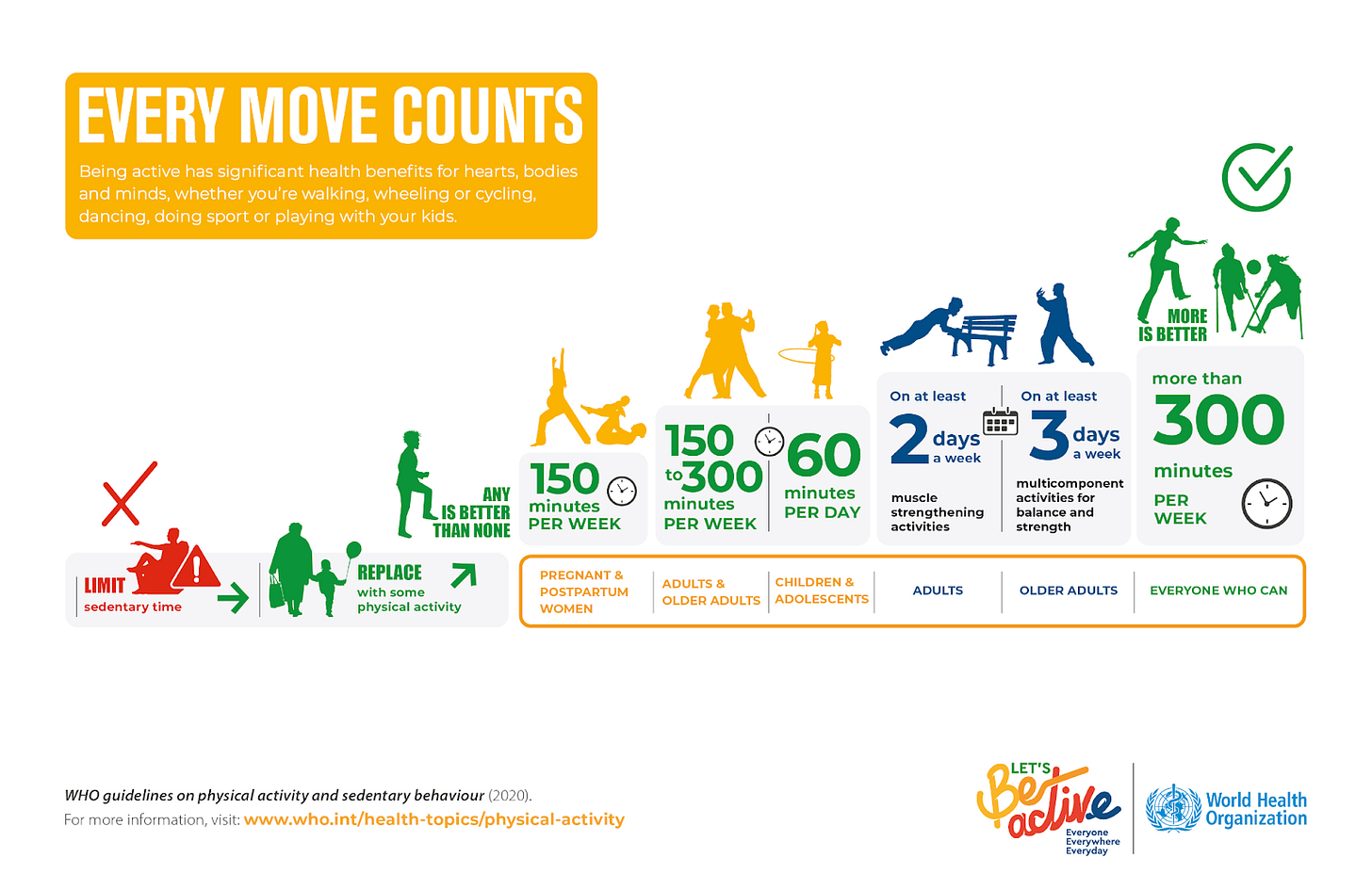
Encourage at least moderate activity, ideally aiming for daily movement per WHO guidelines.
3. Incorporate physical activity into treatment plans
Emphasize physical activity as a fun, low-burden intervention
Discuss it as a tool for emotion regulation, not just fitness.
4. Refer and connect to community resources
Maintain a list of local programs that offer:
Low-cost or free recreational sports
Structured after-school activities
5. Monitor change over time
Track both emotional dysregulation symptoms and physical activity habits as part of ongoing care.
Consider using brief check-ins or follow-up forms completed by caregivers or teachers.
6. Provide psychoeducation and engage families in the rationale
Explain the research-backed link between physical activity and emotional regulation.
Frame physical activity as a skill-building opportunity that helps with focus, mood, and social skills.
This study makes one thing clear: emotional dysregulation can be a key part of ADHD. It also shows that regular physical activity, while it may not replace treatment, can help support emotional regulation. For clinicians, asking about movement and encouraging daily activity can be a small but powerful tool in managing ADHD.
Attribution: This summary was created by the team at Psychvox and is based on insights from the articles:
“The role of physical activity in the association between ADHD and emotional dysregulation” by Narda Ontiveros and colleagues
“Associations Between Physical Activity and Symptoms of Mental Health Disorders in Adolescence: Evidence From the Longitudinal Swedish Twin Register” by Camilla Wiklund and colleagues
All rights to the original research remain with the authors and the publisher. This summary is intended for educational purposes only and does not imply endorsement by the original authors.