Diagnosing on a Spectrum: When Schizotypal Disorder Becomes Schizophrenia
How schizotypal disorder can signal the onset of more serious psychotic conditions
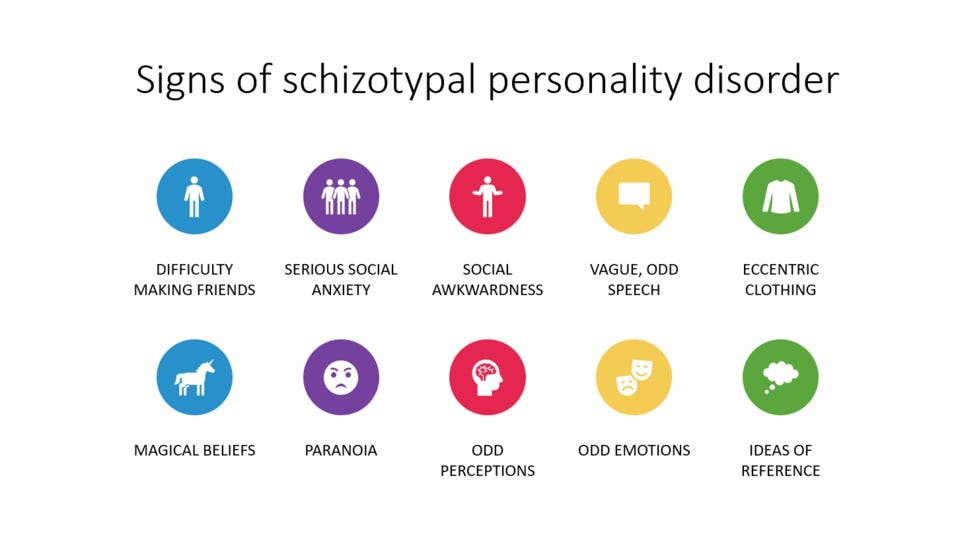
Schizotypal disorder, known as Schizotypal Personality Disorder in the DSM, is a mental health condition that can affect how a person thinks, feels, and interacts with others. People with this disorder often:
Feel very uncomfortable in social situations and struggle to form close relationships
Have unusual or magical beliefs (like telepathy or superstitions)
Show limited or flat emotional expression
Speak in ways that are vague, overly elaborate, or hard to follow
Behave in ways that others might find odd or eccentric
Often feel suspicious or mistrustful of others, even without clear cause
While people with schizotypal disorder usually don’t experience full-blown delusions or hallucinations, their symptoms can sometimes signal the early stages of a more serious mental illness.
Although the DSM classifies it as a personality disorder, many mental health professionals view schizotypal disorder as part of the schizophrenia spectrum. That’s because some individuals eventually go on to develop full psychotic conditions, including schizophrenia.
Recognizing this early phase matters. It offers a potential window to intervene before symptoms become more severe and harder to treat.
How often do people transition from Schizotypal Disorder to psychotic disorders like schizophrenia?
A new nationwide study from Sweden helps clarify just how often that progression happens. Published in Psychiatry Research, the study analyzed data from over 667 adults in Sweden diagnosed with schizotypal disorder between 2006 and 2017. They followed these individuals for up to 12 years using national health and mortality databases.
Here’s what they found:
12.0% of people diagnosed with schizotypal disorder eventually went on to develop schizophrenia.
22.5% of individuals with schizotypal disorder developed other non-affective psychotic disorders, such as delusional disorder, brief psychotic disorder, shared psychotic disorder, or schizoaffective disorder.
About 1 in 3 people who developed schizophrenia did so within the first year of getting diagnosed with schizotypal disorder. The same was true for those who transitioned to other psychotic disorders.
Certain factors made it more likely for someone to develop a more serious psychotic disorder.
Clients without anxiety or depression: Surprisingly, having a history of anxiety or depression appeared to protect against progression to schizophrenia.
Those with comorbid substance use (excluding alcohol): This group was significantly more likely to transition to non-affective psychotic disorders.
In short, not all schizotypal disorder diagnoses carry the same level of risk. The results also highlight that Schizotypal disorder isn’t just an odd or quirky diagnosis: it’s often an early warning sign.
Clinical Takeaways
Expect diagnostic evolution: Schizotypal disorder is fluid and may evolve over time. An initial presentation that fits schizotypal disorder may later meet full criteria for schizophrenia as symptoms worsen. It’s important to treat early diagnoses as provisional and to remain open to re-evaluating them as new information emerges.
Monitor closely in the first 5 years: Most transitions to schizophrenia or other psychotic disorders occurred within the first five years. Establish regular follow-ups during this critical window. Incorporate tools like the Personality Inventory for DSM-5 (PID-5) to measure symptom dimensions beyond categorical labels.
Screen for early signs of psychosis: Use tools like the Structured Interview for Psychosis-Risk Syndromes (SIPS) or the Comprehensive Assessment of At-Risk Mental States (CAARMS) to monitor clients with schizotypal traits for emerging psychotic features.
Assess substance use carefully: Non-alcohol substance use was associated with a higher risk of transition. Incorporate routine substance use screenings (e.g., DAST-10, AUDIT) into your assessment plan.
Educate and involve families early: Family members often notice subtle shifts first. Use psychoeducation and shared decision-making to help them support early identification and intervention.
Document changes clearly: When diagnostic reclassification happens, make sure your notes reflect why and how the clinical picture evolved. This helps ensure continuity of care and guides future treatment planning.
Attribution: This summary was created by the team at Psychvox and is based on insights from the articles “Transition from schizotypal disorder to non-affective psychotic disorders including schizophrenia: A nationwide Swedish cohort study” by S. Lindström and colleagues. All rights to the original research remain with the authors and the publisher. This summary is intended for educational purposes only and does not imply endorsement by the original authors. The articles are licensed under the Creative Commons Attribution 4.0 International License (CC BY 4.0).