Rethinking Mood Disorders in Menstruating Patients
New research highlights how mood and physiology shift across the menstrual cycle in women with depression
Note: We refer to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision as the DSM. Acronyms used in this article include:
PMDD: Premenstrual Dysphoric Disorder
PME: Premenstrual Exacerbation
PMS: Premenstrual Syndrome
HRV: Heart Rate Variability
“"Premenstrual exacerbation of depression is present in women with depression, similar to the pattern seen in premenstrual dysphoric disorder."
For many women, mood changes before a period are an inconvenience. But for others, these shifts are profound, disrupting work, relationships, and overall mood and mental stability.
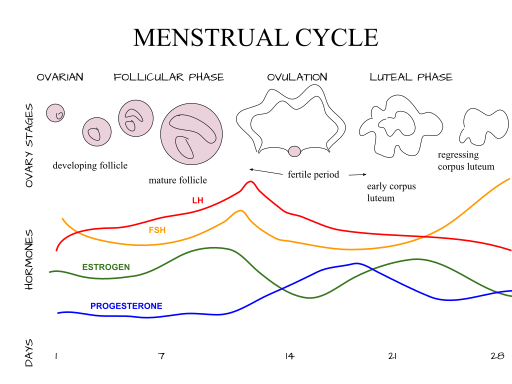
Premenstrual Dysphoric Disorder (PMDD), now classified in the DSM as a depressive disorder, and Premenstrual Exacerbation (PME), a less-recognized clinical pattern, reveal just how much we still need to understand about mood fluctuations across the menstrual cycle.
PMDD, PMS, and PME: What’s the Difference?
Premenstrual Dysphoric Disorder (PMDD) is a hormone-related mood disorder that affects about 1.6% of people. It causes emotional symptoms like mood swings, irritability, and anxiety. These symptoms usually start in the two weeks before a period and improve once the period begins. To be diagnosed, symptoms must:
Happen in most cycles over the year
Seriously affect daily life
Include at least one mood-related symptom, such as mood swings
Premenstrual syndrome (PMS) also includes the presence of symptoms such as low mood in the luteal phase. However, PMS is more common and typically milder, lacking the severe emotional and functional disruptions of PMDD.
PMS is believed to affect 47% of the world’s female population.
Premenstrual Exacerbation (PME) is different still. It refers to the worsening of an existing condition, like major depressive disorder (MDD), during the premenstrual phase. Unlike PMDD, PME is not a diagnosis in itself but a cyclical pattern observed within another disorder. Some studies suggest that up to 80% of women with psychiatric disorders may have PME.
When assessing premenstrual mood symptoms, it’s essential to distinguish PMDD and PME from other conditions. Here's how:
Major Depressive Disorder (MDD):
PMDD and PMS are cyclical, with symptoms tied specifically to menstrual phases. In contrast, Major Depressive Disorder is persistent, with mood symptoms present throughout the menstrual cycle
PME refers to the worsening of an existing disorder, like MDD, in the premenstrual window
PME may mimic PMDD patterns, but it occurs in individuals already diagnosed with depression
Hormonal Treatments and Contraceptive Use:
Hormonal contraception has variable effects: some studies show it improves PMD symptoms, others show no change or even worsening of depression
The study noted similar rates of PME in women with and without hormonal contraception, suggesting it’s not solely hormonally driven
Notably, women on Selective Serotonin Reuptake Inhibitors still experienced PME
Other Mood Disorders (e.g., Bipolar Disorder):
Bipolar mood fluctuations can also follow cyclical or seasonal patterns, but require very different treatment approaches
Clinicians should be careful not to confuse PME with mood changes from bipolar disorder, especially when symptoms get worse before a period.
New Insights
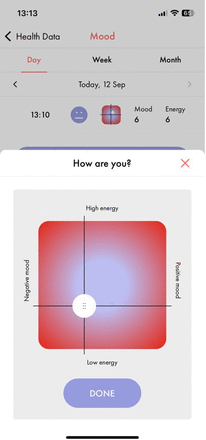
A 2025 study by Delray et al. offers critical insights. Using tools such as Juli, a health app available on iOS and Android, researchers tracked mood, energy, heart rate variability (HRV), and menstrual cycle phases in 352 women with diagnosed depression.
The study yielded some key findings regarding premenstrual exacerbation (PME) in women diagnosed with depression:
Mood decline began up to 14 days before menstruation, with the lowest ratings observed from 3 days before through 2 days after menses.
More than half of the women (54%) showed this pattern, confirming a high prevalence of PME in this population.
Heart rate variability (HRV), a possible marker for mood, was tightly linked to these fluctuations, tracking daily mood shifts even with up to a three-day lag.
Energy levels, however, remained stable, suggesting that fatigue may not be a distinguishing symptom of PME in women already experiencing depression.
Why PME Matters Clinically
PME carries significant treatment implications. Research has linked PME with treatment resistance, a chronic illness course, and lower functioning. Yet many clinicians still conflate PME with PMDD, potentially leading to inappropriate treatment strategies.
Prospective symptom tracking, especially through mobile apps that capture daily fluctuations and physiological markers, can help distinguish PME from PMDD. In this study, symptom patterns were only observable when tracked across at least two full cycles, underscoring the importance of longer-term data.
The Takeaway for Clinicians
This study makes a compelling case: we must take menstrual cycle-related mood shifts seriously in depression treatment.
Ask about cycle-related changes. Don’t assume mood symptoms are constant. Ask patients with depression if they notice changes in mood, energy, or sleep in the days leading up to their period.
Use validated tools such as the Premenstrual Symptom Screening Tool (PSST) in diagnosis. Learn more about the disorders and different ways to evaluate them here.
Encourage daily mood tracking over at least two full cycles to help document and validate symptom patterns. While a paper calendar works, digital tools often make tracking easier. Recommend apps like Juli, which let patients track mood, energy, and their menstrual cycle all in one place, making it easier to spot patterns that might otherwise be missed.
Don’t overlook the timing. If a patient’s depression worsens just before their period, consider whether Premenstrual Exacerbation (PME) may be at play, even if they don’t meet criteria for PMDD. This distinction matters for treatment planning.
Adjust treatment to fit the pattern. If you notice a consistent premenstrual drop in mood, you may need to adapt the treatment plan. This could mean adjusting medication timing, considering hormonal influences, or supporting the patient through high-risk days.
Understanding how the menstrual cycle affects mood is essential for better care. For many patients with depression, these fluctuations are real, disruptive, and too often dismissed. By asking the right questions and using the right tools, clinicians can uncover patterns that unlock more effective, personalized treatment.
Attribution: This summary was created by the team at Psychvox and is based on insights from the article “Tracking mood symptoms across the menstrual cycle in women with depression using ecological momentary assessment and heart rate variability” by Kyra Delray and colleagues. All rights to the original research remain with the authors and the publisher. This summary is intended for educational purposes only and does not imply endorsement by the original authors. The article is licensed under the Creative Commons Attribution 4.0 International License (CC BY 4.0).