The Cost of Silence: Why OCD Goes Untreated for Years
New research reveals how delayed help-seeking and misunderstood symptoms shape outcomes in obsessive-compulsive disorder
"“Sexual OCD” and “Harm OCD”, involving intrusive and unwanted sexual and violent thoughts, images, and urges, are terrifying experiences for the person, that may be worried about explaining these symptoms and burdened by the guilt the thoughts might cause."
"It is now clear, from several individual studies, that a long duration of untreated illness is a negative prognostic factor and is responsible for treatment resistance."
"...as the disorder remains untreated, the compulsive behaviours could become habitual in nature and could develop as habits or automatic rituals, apparently no longer linked with obsessions; this could make the OCD more difficult to treat."
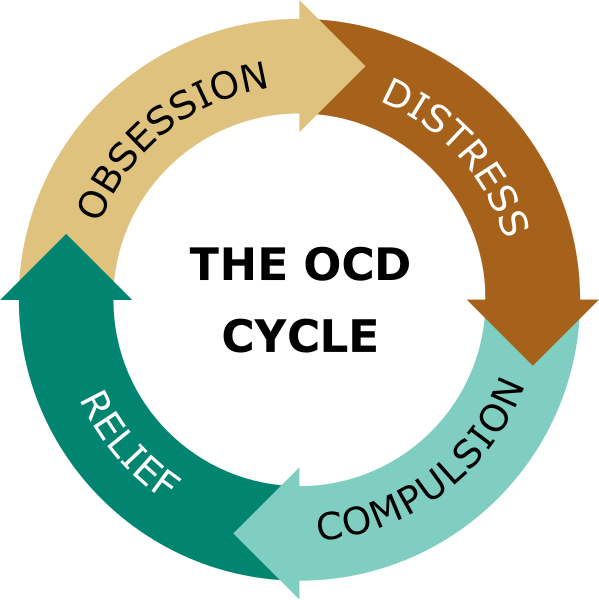
Obsessive-compulsive disorder (OCD) is a mental health condition marked by intrusive, distressing thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions) performed to reduce anxiety or prevent imagined harm. These cycles can become so time-consuming or overwhelming that they interfere with daily life, work, and relationships.
The illness affects about 1.2% of the U.S. population each year, with symptoms typically beginning around age 19. For boys, however, symptoms can often begin in childhood. While the disorder usually develops gradually, it can sometimes appear suddenly.
While the specific content of obsessions and compulsions can vary, ranging from fears of contamination to needing things to feel “just right”, what unites them is the intense discomfort they cause and the urgency to neutralize that discomfort.
And although effective treatments for OCD exist, a substantial portion of individuals still go without care. Global estimates suggest that nearly half of those with OCD never seek treatment, and in some studies, as many as 90% report receiving no professional guidance whatsoever. Beyond the lack of professional help, misdiagnosis remains a major barrier, often delaying or preventing access to appropriate, evidence-based treatment.
Barriers to treatment and care
An article published in 2013 revealed a striking gap in clinicians’ ability to recognize certain forms of OCD, particularly those involving taboo thoughts. In a national survey of licensed psychologists, 77% misidentified a vignette describing sexual orientation-related obsessions as “sexual identity confusion” rather than OCD. These findings highlight how even well-trained professionals often overlook or misunderstand less visible forms of OCD.
This barrier contributes to what researchers call the duration of untreated illness (DUI): the time between when OCD symptoms first appear and when someone finally receives proper treatment. Studies show this delay often lasts between 7 and 8 years, and sometimes even longer.
This matters because the longer OCD goes untreated, the harder it can be to treat. Over time, compulsions can become automatic habits, less connected to the original fears and harder to interrupt. Early treatment not only improves outcomes, but it may also prevent the disorder from becoming more deeply ingrained and resistant to change.
To better understand how long people with OCD typically wait before getting help, researchers conducted a meta-analysis to calculate the average age at help-seeking and the average duration of untreated illness. They also explored what factors might influence these delays, given the wide variation seen across individual studies.
Researchers found that people with OCD often wait years before getting help. On average, they first seek treatment around age 29, nearly seven years after symptoms begin. This long delay can make the disorder harder to treat and is linked to worse outcomes.
The type of symptoms also affects how soon someone seeks help. People with visible behaviors, like constant checking, tend to get help earlier. But those with more private or distressing thoughts, such as fears of harming others or sexual obsessions, often delay, driven by fear, shame, or worry about being misunderstood. These delays highlight the urgent need for greater public awareness and better clinician training to recognize OCD in all its forms.
Clinical Takeaways
Recognize the Cost of Delay: On average, people with OCD seek help nearly 7 years after symptoms begin, often around age 29. This long duration of untreated illness (DUI) is a major risk factor for worse outcomes, treatment resistance, and even suicide. Clinicians should treat DUI as a modifiable target for early intervention.
Symptom Type Affects Timing: The type of OCD symptoms that show up can significantly influence how soon individuals seek help.
Visible compulsions, such as checking locks, appliances, or seeking reassurance, are easier to recognize and more commonly associated with OCD. Because they are outwardly observable and often discussed in public or clinical settings, these symptoms can lead to earlier care.
Taboo obsessions include intrusive, unwanted thoughts about:
Harming others (e.g., fear of stabbing someone)
Sexual images or urges (e.g., involving children or inappropriate contexts)
Religious violations (e.g., thoughts of disrespecting sacred symbols)
These obsessions are deeply distressing and often misunderstood, leading to shame, fear of judgment, or misdiagnosis. As a result, individuals with these symptoms are more likely to delay seeking help.
Somatic obsessions involve an intense preoccupation with the body or fears of having a serious illness (e.g., obsessive focus on heartbeat, breathing, or a perceived undiagnosed condition). These can lead to avoidance of medical settings or confusion over whether symptoms are physical or psychological, further delaying care.
Clinicians should be proactive in asking specific, nonjudgmental questions to uncover these less visible, but highly impairing, symptom types. A broad and open clinical inquiry is key to early identification and effective treatment
Use Validated Screening Tools:
The Yale-Brown Obsessive Compulsive Scale (Y-BOCS) remains a gold-standard tool for assessing symptom type and severity.
Consider using disorder-specific tools like the Dimensional Obsessive-Compulsive Scale (DOCS) to better capture a range of symptom presentations.
Educate with Compassion: Psychoeducation should directly address shame and fear, especially around intrusive thoughts. Normalize the experience of unwanted thoughts and help clients to understand the difference between obsessions and desires or intentions.
The International OCD Foundation (IOCDF) offers clinician handouts, training programs, and patient education materials (link here)
Attribution: This summary was created by the team at Psychvox and is based on insights from the article “Meta-analysis of age at help-seeking and duration of untreated illness (DUI) in obsessive-compulsive disorder (OCD): The need for early interventions” by Luca Pellegrini and colleagues. All rights to the original research remain with the authors and the publisher. This summary is intended for educational purposes only and does not imply endorsement by the original authors. The article is licensed under the Creative Commons Attribution 4.0 International License (CC BY 4.0).