Treating Insomnia to Relieve Depression
A new trial shows promising improvements in sleep and mood
[Note: Above is an AI-generated read-through of the text summary below, so that you can listen to it on the go]
Another note: We reached out to the team at somnio, the app that we mention below. Unfortunately, the app is only available in the German Market at this time. You can learn more about a similar app, SleepioRx, in the United States here. The app can be found here.
Mental health disorders are typically defined by their core symptoms—but these disorders can show up in unexpected ways that differ from common perceptions.
Anxiety Disorders
While we often associate anxiety primarily with excessive worry, it can also manifest as:
Difficulty breathing
Chest pain
Nausea
Fear of losing control
Hot flashes
Irritability
Difficulty concentrating
Schizophrenia
Most people think of hallucinations or delusions, but symptoms can also include:
Difficulty staying on topic (disorganized thinking)
Lack of motivation (avolition)
Reduced emotional expression (flat affect)
Depression can follow a similar pattern.
When envisioning depression, we picture someone struggling with a loss of interest, motivation, and persistent and repetitive difficult thoughts. However, a lesser-known yet profoundly impactful symptom is sleep disturbance, particularly insomnia.
In fact, approximately 85% of individuals with depression meet the diagnostic criteria for insomnia disorder, which includes difficulties falling or staying asleep, persistent fatigue, daytime sleepiness, irritability, and impaired concentration. An astonishing 93% report experiencing at least some insomnia-related symptoms.
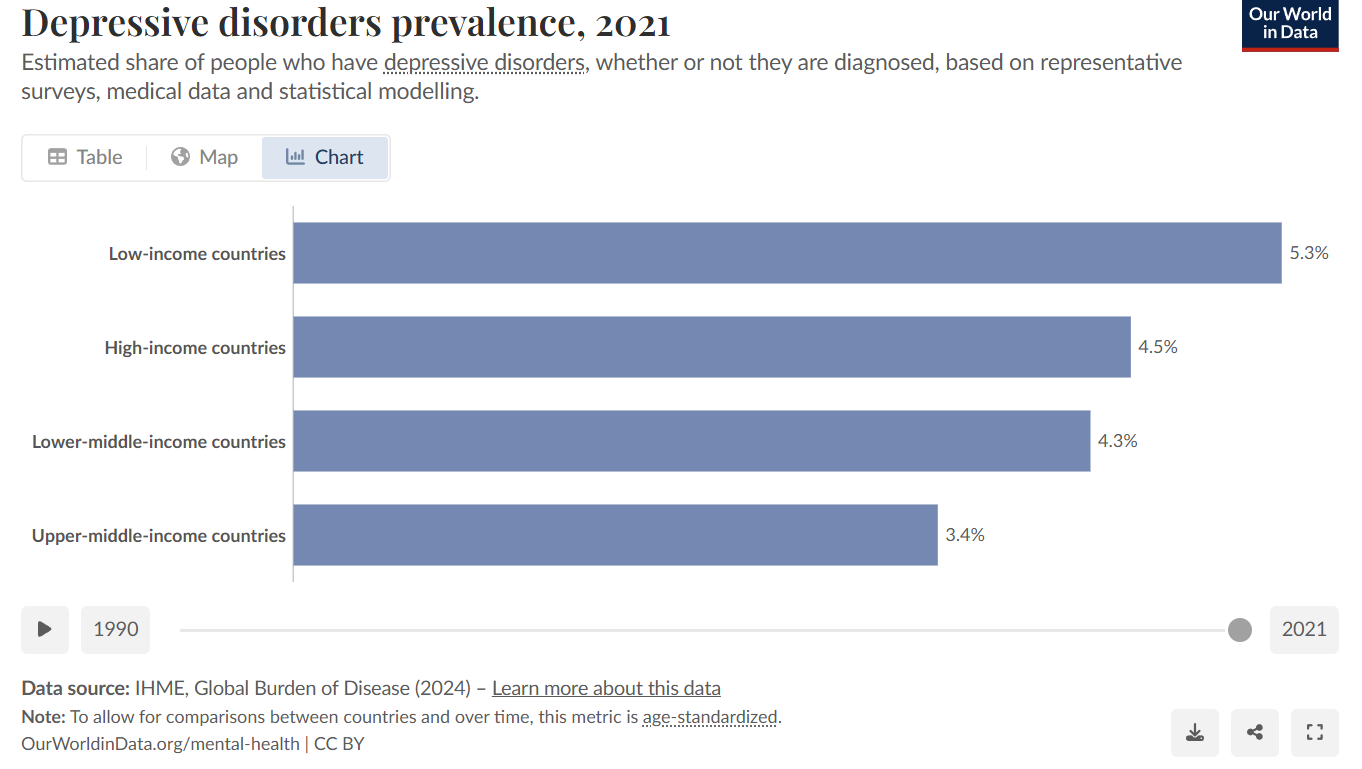
Depression affects between 3% and 5% of people in the world and has a high rate of relapse, with severity and risk increasing after each episode.
The relationship between depression and insomnia is bidirectional—each can worsen or improve the other. And research suggests that insomnia disorder cuts across multiple mental health diagnoses. It’s not tied to just depression, but can show up in other disorders such as anxiety.
Additionally, insomnia disorder can arrive before a depression diagnosis and worsen symptoms such as emotional distress, the inability to experience pleasure or enjoyment, mental or physical fatigue and motivation, concentration problems, and suicidality.
Clinical studies show that people with worse insomnia at the start of depression treatment tend to have poorer outcomes. Even when depression improves, insomnia often sticks around—and it can be a reason for why a person relapses.
Fortunately, insomnia can be directly addressed through intervention. And treating insomnia alongside depression can boost treatment success and lower the chance of depression coming back.
A digital tool for insomnia
One of the first-line treatments for treating insomnia is Cognitive Behavioral Therapy for Insomnia (CBT-I). This is also a supported treatment for depression when antidepressants are not suitable due to side effects.
A recent study conducted in Germany examined whether incorporating a digital CBT-I program into existing treatments could improve outcomes for both depression and sleep disturbances. But what exactly is digital CBT-I? It refers to a digital health application specifically designed to address sleep difficulties, such as insomnia.
One such application is Somnio, which is recognized as a primary treatment option for adult insomnia by the German Sleep Society. In Germany, physicians and psychotherapists can prescribe Somnio, and its costs may be covered by insurance, making it an accessible intervention for those struggling with sleep disorders.
The app consists of ten core modules based on elements of standard therapy including psychoeducation, relaxation techniques, and cognitive therapy. It has an interactive avatar that guides the user, and the app attempts to increase engagement by sending notifications and reminders.
The Study at a Glance
Conducted in Germany and published in Depression and Anxiety (2025), this randomized controlled trial recruited 140 adults with clinically diagnosed depression and insomnia. Below, you will see the term “care-as-usual”, which means that the participant in the trial continued with their standard treatment during the trial. In other words, if a person was on medication and/or seeing a mental health therapist, they continued with that throughout the trial.
Participants in the trial were assigned to either:
Somnio + Care-as-Usual (CAU)
Waitlist Control (WLC) + CAU: No Somnio access for 24 weeks.
The results were measured using the patient health questionnaire-9 scale, better known as the PHQ9, which is a tool used to measure the severity of depression. Insomnia was measured through the Insomnia Severity Index.
Key Findings: The Highlights
Depressive Symptoms Improved
After 12 weeks, those using Somnio saw an average drop of 3.34-points on the PHQ-9, compared to the people who did not use the app. And after 24 weeks, this drop was on average 2.83 points lower between the groups.
Around 30% of participants had a 50% or greater reduction in symptoms, and 5.7% reached full remission, or recovery. Only 1.4% of those in the control group achieved remission. However, these results may have been due to random chance. Nevertheless, it may be something worth paying attention to, especially as a treatment to a treatment resistant population.
Sleep Also Improved—Big Time
Insomnia symptoms decreased significantly and sustainably for those using somnio right after treatment at the 12 week mark and even 3 months later, at the 24 week mark.
The research called the people who got much better responders. In terms of insomnia, responders were defined as people who had an 8 point drop on the Insomnia Severity Index or greater. At 12 weeks, 50% of people who used somnio improved this much, compared to only 5.71% of those in the control group not using the app. And at 24 weeks, 34% of those using the app were still responders, compared to 14% in the control group.
In terms of remission, or when symptoms are essentially gone, at 12 weeks, 18% of people using the app were in remission compared to 0% of people not using the app. And at 24 weeks, 11.4% of people were still in remission, compared to 5.7% of people in the control group.
People using the app also showed reduced fatigue and increased well-being.
Daytime sleepiness and the time it takes a person to fall asleep after going to bed did not significantly improve.
Therapist Takeaways
Sleep Isn’t Just a Symptom—It’s a Treatment Target
Insomnia and depression are deeply intertwined. Insomnia can precede depression, worsen its symptoms, and linger even after mood improves. Addressing sleep problems directly can enhance depression treatment outcomes—and may even reduce relapse risk. Don't wait for sleep to improve on its own.
Digital CBT-I is effective and scalable.
Digital CBT-I (like somnio) significantly reduced both insomnia and depressive symptoms—even in individuals already receiving care-as-usual (meds, therapy, or both). This makes it a compelling add-on treatmentDigital CBT-I does not address every symptom. For example, while fatigue improved, daytime sleepiness did not. This distinction is important to consider during treatment. A client may report feeling more energized and less fatigued, yet their experience of daytime sleepiness may remain largely unchanged.
Broader Mental Health Benefits Are Real
Beyond sleep, dCBT-I also improved:
Overall well-being
Positive mood (affect)
Negative mood
Rumination
Engagement Can Be a Barrier—Plan Ahead
Only about 1 in 3 participants completed all 10 modules, though two-thirds completed at least half. That’s a solid starting point, but dropout is a known challenge in digital interventions.Therapist strategies:
Help clients set realistic goals (e.g., one module/week)
Normalize setbacks in sticking to treatment
Use brief check-ins to reinforce progress and troubleshoot challenges
Even partial completion can lead to meaningful gains.
6. Bring CBT-I Into the Therapy RoomEven if clients aren’t using a digital app, you can still apply core CBT-I components:
Sleep restriction
Stimulus control (bed = sleep only!)
Cognitive restructuring around unhelpful sleep beliefs
Psychoeducation on sleep cycles and habits
In conclusion, sleep isn’t just a side quest: it’s a main character in depression treatment. Digital CBT-I offers a powerful, accessible way to improve both sleep and mood. Whether you're referring clients to an app or weaving CBT-I into your sessions, sleep deserves a front-row seat in therapy planning for depression.
Attribution: This summary was created by the team at Psychvox and is based on “Digital CBT-I in Comorbid Insomnia and Depression: Clinical Outcomes From a Pragmatic Randomized Controlled Trial” by Jennifer Schuffelen and colleagues. The article is licensed under CC BY 4.0. Changes were made to adapt the content for clarity, style, and length. No additional restrictions have been applied, and nothing in this summary should be taken to imply endorsement by the original authors.